What Is Cervical Cancer?
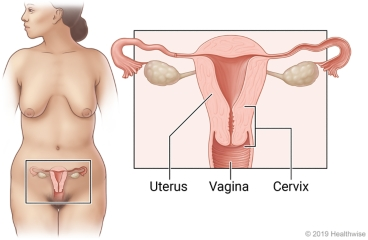
Cervical cancer develops when cells in the cervix, which is the lowest part of the uterus, begin to grow out of control. These cells can also invade nearby tissues or spread throughout the body. Usually, cervical cancer is very slow-growing. However, in certain circumstances, it can grow and spread quickly.
The most common type of cervical cancer is called squamous cell carcinoma. The second most common form is adenocarcinoma. It comes from cells that make up glands in the cervix. There are a few other very rare types like small cell and neuroendocrine carcinoma, but they are extremely uncommon.
What causes cervical cancer and am I at risk?
Cervical cancer is much more common in developing nations than it is in developed nations and is fairly rare in the United States. Every year, an estimated 13,800 cases of cervical cancer are diagnosed in the United States. There has been a 75% decrease in deaths from cervical cancer in developed nations over the past 50 years. Most of this decrease is attributed to the effective institution of cervical cancer screening programs (HPV testing and/or Pap testing).
One of the most important risk factors for cervical cancer is infection with a virus called HPV (human papillomavirus). Most persons will be exposed to HPV at some point in their lifetime, but only a very small percentage who have HPV will develop cervical cancer. Just because you have HPV doesn’t mean you will get cancer. However, almost all cervical cancers have evidence of the HPV virus in them, so HPV infection is a major risk factor for developing it. HPV is a sexually transmitted infection (STI) that is incredibly common in the population.
HPV is the virus that causes genital warts, but having genital warts doesn’t necessarily mean you are going to get cervical cancer. There are different subtypes, or strains, of HPV. Only certain subtypes are likely to cause cervical cancer. Often, infection with HPV causes no symptoms at all, until a woman develops a pre-cancerous lesion of the cervix which can be detected on exam and/or pap smear.
Because having an STI is a risk factor for cervical cancer, any risk factor for developing STIs is also a risk factor for developing cervical cancer. These include:
–Having had multiple male sexual partners.
–Starting to have sexual intercourse at an early age.
–Having had male sexual partners who are considered high risk (they have had many sexual partners and/or began having sexual intercourse at an early age).
–Being diagnosed with any other sexually transmitted diseases (like herpes, gonorrhea, syphilis, or Chlamydia).
–HIV infection is another risk factor for cervical cancer, but for a slightly different reason. It appears that any condition that weakens your immune system also increases your risk for developing cervical cancer.
Another important risk factor for developing cervical cancer is smoking. Smokers are at least twice as likely as non-smokers to develop cervical tumors.
How can I prevent cervical cancer?
There are several things one can do to decrease the risk of getting cervical cancer. This includes:
Have regular screenings: The drastic drop in cervical cancer cases and deaths in the United States has been because of HPV and Pap testing.
Get vaccinated:
Three vaccines, called Gardasil, Gardasil 9, and Ceravix have been developed. Currently, only Gardasil 9 is available in the US.
The HPV vaccine is recommended for all individuals aged 12-26. The US FDA has approved the vaccine for use up to age 45, however, not all insurance companies cover the HPV vaccine for individuals over the age of 26.
These vaccines have been demonstrated to be effective in preventing infection with some strains of HPV if they are given before a person is exposed to HPV. Even if you already have HPV, you can still be vaccinated. The vaccine can protect you from other types of HPV.
In addition to cervical cancer, HPV is also a cause of vulvar, vaginal, penile, and anal cancers and some head & neck cancers. It also causes genital warts and leads to abnormal Pap test results that result in further testing or treatment.
Don’t start smoking, and if you are already a smoker, it is time to quit. Smoking has been shown to decrease the immune system’s ability to clear an HPV infection.
People can limit their numbers of sexual partners, and delay the onset of sexual activity to reduce risk, as more partners can increase the likelihood of infection. Using condoms may decrease areas that are exposed but cannot prevent exposure entirely.
What are the signs of cervical cancer?
The early stages of cervical cancer usually do not have any symptoms. This is why it is important to have screening Pap tests. As a tumor grows in size, it can produce a variety of symptoms including:
–Abnormal bleeding (including bleeding after sexual intercourse, in between periods, heavier/longer lasting menstrual bleeding, or bleeding after menopause).
–Abnormal vaginal discharge (may be foul-smelling).
–Pelvic or back pain.
–Pain with urination.
–Blood in the stool or urine.
–Pain during sex.
Many of these symptoms are non-specific and can represent a variety of different conditions. If you have any of these symptoms, talk with your healthcare provider.
How is cervical cancer diagnosed?
The most common reason for your provider to pursue the diagnosis of cervical cancer is if you have an abnormal HPV and/or Pap test. Remember these tests are screening tests, not diagnostic. Further testing after an abnormal result is needed.
Pap tests help find pre-cancerous lesions in your cervix. A pre-cancerous lesion means that there are abnormal appearing cells, but they haven’t invaded past a tissue barrier in your cervix; thus a pre-cancerous lesion cannot spread or harm you. However, if left untreated, a pre-cancerous lesion can evolve into invasive cancer.
After getting an abnormal pap smear, your provider may recommend a colposcopy, which is a procedure done during a pelvic exam with the aid of a colposcope (which is like a microscope). By using acetic acid on the cervix and examining it with a colposcope, your provider can look for abnormal areas of your cervix. Colposcopy is uncomfortable, but not painful, and can be done in your gynecologist’s office. If there are any abnormal areas, a biopsy may be obtained. A biopsy is the only way to know for sure if you have cancer.
How is cervical cancer staged?
FIGO Surgical Staging of Cervical Cancer (2018)
|
FIGO Stage |
Description |
|
I |
Cervical carcinoma confined to the cervix |
|
IA |
Invasive carcinoma diagnosed only by microscopy. Stromal invasion with a maximum depth of ≤5.0mm |
|
IA1 |
Measured stromal invasion of ≤3.0mm or less in-depth |
|
IA2 |
Measured stromal invasion >3.0mm and ≤5.0mm |
|
IB |
Invasive carcinoma with measured deepest invasion >5 mm (greater than stage IA); lesion limited to the cervix uteri with size measured by maximum tumor diameter. |
|
IB1 |
Invasive carcinoma >5mm depth of stromal invasion and ≤2cm in greatest dimension |
|
IB2 |
Invasive carcinoma >2cm and ≤ 4cm in greatest dimension |
|
IB3 |
Invasive carcinoma >4cm in greatest dimension |
|
II |
Cervical carcinoma invading beyond the uterus but not extended onto the lower third of the vagina or to the pelvic wall |
|
IIA |
Involvement limited to the upper two-thirds of the vagina without parametrial invasion. |
|
IIA1 |
Invasive carcinoma ≤4cm in greatest dimension |
|
IIA2 |
Invasive carcinoma >4cm in greatest dimension |
|
IIB |
Parametrial invasion but not up to the pelvic wall |
|
III |
The carcinoma involves the lower third of the vagina and/or extends to the pelvic wall and/or causes hydronephrosis or non-functioning kidney and/or involves pelvic and/or paraaortic lymph nodes |
|
IIIA |
Tumor involving the lower third of the vagina but no extension to the pelvic wall |
|
IIIB |
Carcinoma involves the lower third of the vagina, with no extension to the pelvic wall |
|
IIIC |
Involvement of pelvic and/or paraaortic lymph nodes (including micrometastases), irrespective of tumor size and extent |
|
IIIC1 |
Pelvic lymph node metastasis only |
|
IIIC2 |
Paraaortic lymph node metastasis only |
|
IV |
The carcinoma has extended beyond the true pelvis or has involved (biopsy-proven) the mucosa of the bladder or rectum. |
|
IVA |
Spread of the growth to adjacent organs |
|
IVB |
Spread to distant organs |
How is cervical cancer treated?
Pre-cancerous lesions
Persons who have pre-cancerous lesions on biopsy after colposcopy have a few different options with how to proceed. You may decide on a specific option depending on whether or not you plan to have children in the future, your current health status and life expectancy, and your concerns about the future and the possibility of having cancer come back. You should talk to your provider about your fears, concerns and preferences.
There are several ways to remove precancerous lesions without removing the entire uterus (and thus preserving your ability to have a baby in the future). Options include:
–Loop electrosurgical excision procedure or LEEP (the same type of electrosurgical procedure used for biopsies).
–Cold knife conization (the thicker type of biopsy that gets tissue under the surface).
Those who do not have any plans to have children in the future and are particularly worried about their chances of getting invasive cancer may elect to have a hysterectomy (a surgery that removes your uterus and cervix). This procedure is more invasive than any of the previously mentioned treatment modalities but can provide peace of mind to those who do not want to have children.
Surgery
Surgery is generally used in early-stage cervical cancers. There are a few different types of surgeries that can be performed. The type of surgery depends on the stage of the tumor. The most common surgical procedures for cervical cancer include:
–Trachelectomy- Removal of the cervix, upper vagina, and tissue surrounding the cervix. Pelvic lymph nodes may also be removed.
–Hysterectomy- Removal of the uterus and cervix. Pelvic lymph nodes may also be removed. Depending on the amount of disease, your provider may have to remove tissues around the uterus, as well as part of the vagina and the fallopian tubes.
One of the benefits of surgery in young persons is that oftentimes their ovaries can be left. This keeps them from going through menopause at an early age. Higher stage disease is usually treated with radiation and chemotherapy.
Radiation Therapy
Radiation therapy is given under the care of a radiation oncologist, and has been shown to be very effective in treating cervical cancer. Radiation therapy uses high energy x-rays to kill cancer cells. Advanced stage cervical cancer is most often treated with radiation. Radiation can also be used in patients who are too ill to risk having anesthesia/surgery. Radiation has the benefit of being able to treat all of the disease in the radiation field, so that lymph nodes can be treated as well as the primary tumor in the course of the same treatment.
Radiation therapy for cervical cancer either comes from an external source (outside of the patient, known as external beam radiation) or an internal source (inside the patient, known as brachytherapy). The duration of your treatment will be determined by your radiation oncologist. The treatment takes just a few minutes and is painless.
The type of radiation therapy used depends on the stage of your tumor, and is often given in conjunction with chemotherapy. Radiation therapy for cervical cancer either consists of x-rays delivered from the outside of the patient (external beam radiation/EBRT) and/or from a radioactive source placed inside the vagina (brachytherapy). External beam radiation therapy requires patients to come in 5 days a week for up to 6 weeks to a radiation therapy treatment center. The treatment takes just a few minutes, and is painless. Brachytherapy (also called intracavitary irradiation) allows your radiation oncologist to “boost” the radiation dose to the tumor bed. This provides an added impact while sparing your normal tissues. This is done by inserting a hollow tube (that contains a small radioactive source) into your vagina for a few minutes. This type of brachytherapy is called high dose rate (HDR) brachytherapy, and can be performed as an outpatient procedure.
Another use of radiation is in palliative care. In patients with very advanced cases of cervical cancer, the goal of treatment is to ease pain or symptoms, rather than trying to cure their disease.
In any setting, radiation is often combined with chemotherapy, and, depending on your case, your provider will decide with you on the best possible treatment arrangement for your lifestyle and wishes.
Chemotherapy
Despite the fact that tumors are removed by surgery or treated with radiation, there is always a risk of recurrence because there may be microscopic cancer cells left in the body. In order to decrease the risk of a recurrence (the cancer coming back), you may be offered chemotherapy.
Chemotherapy is the use of anti-cancer drugs that go throughout the entire body. Most patients in good medical condition and receiving radiation for stage IIA or higher cervical cancer will be offered chemotherapy in addition to their radiation. There have been many studies that demonstrate the usefulness of adding chemotherapy to radiation in terms of decreasing mortality from cervical cancer.
There are many different chemotherapy drugs, and they are often given in combinations for a series of months. Depending on the type of chemotherapy regimen you receive, you may get medication every week or every few weeks. The most commonly used regimens (combinations) use drugs such as cisplatin, etoposide, paclitaxel, topotecan, carboplatin and/or bevacizumab. Cisplatin is often given weekly at the same time as radiation treatment.
Other drugs such as pembrolizumab, albumin-bound paclitaxel, docetaxel, fluorouracil, gemcitabine, ifosfamide, irinotecan, mitomycin, pemetrexed, and vinorelbine may be used as second-line therapy after recurrence.
Follow-up Care and Survivorship
Once you have been treated for cervical cancer, you need to be closely followed for a recurrence. At first, you will have follow-up visits fairly often. The longer you are free of disease, the less often you will have to go for checkups. Your provider will tell you when they want follow-up visits, Pap tests, and/ or scans depending on your case. Your provider will also do pelvic exams regularly during your office visits. It is very important that you let your provider know about any symptoms you are experiencing and that you keep all of your follow-up appointments.
Fear of recurrence, relationships and sexual health, the financial impact of cancer treatment, employment issues, and coping strategies are common emotional and practical issues experienced by cervical cancer survivors. Your healthcare team can identify resources for support and management of these challenges faced during and after cancer.
Resources for More Information
National Cervical Cancer Coalition
Provides education about HPV and cervical cancer, support through a “pals” program that links a woman with another woman who has a similar diagnosis.
Foundation for Women’s Cancers
The Foundation offers comprehensive information by cancer type that can help guide you through your diagnosis and treatment. They also offer the ‘Sisterhood of Survivorship’ to connect with others facing similar challenges.
Hope for Two
Dedicated to providing those diagnosed with cancer while pregnant with information, support, and hope.
Chemocare
Provides information and resources about chemotherapy drugs.
Sharp Hospital Cancer Support Groups and ServicesSharp offers a comprehensive range of support services to help you and your loved ones manage your cancer diagnosis and treatment.
Scripps Cancer Support Groups and Services
Scripps MD Anderson offers an array of cancer support programs, services and resources to help you every step of the way.
References
All About Cervical Cancer | OncoLink